
Στήθος (8)
General
Nowadays, breast augmentation is among the most popular procedures in plastic surgery.
Breasts have always been considered as one of the stronger features of femininity. Therefore, women whose breasts are not of what is considered to be the right size, may often feel less favoured compared to other women in terms of femininity. They may also feel inferior to other women. This often reflects on their overall behaviour and personality. These women may have small or aplastic breasts, breast asymmetry or maybe they’ve undergone a mastectomy. A breast augmentation procedure helps fix these problems.
Which are the breast augmentation techniques used in modern plastic surgery?
- Non touch - No pain Technique
- Dual plane technique
- Subfascial technique
What can we promise? What are we aiming for?
Our aim is to increase breast volume using silicone implants in such a way as to obtain a natural result in harmony with the patient's body features.
Nevertheless, new techniques used in breast augmentation and the methods we suggest for achieving the most natural results are: the subfascial technique where the implant is placed under a thin membrane that covers the muscle, called fascia, and the “Dual plane technique” where the implant is inserted half under the muscle and half under the muscle fascia.
10 facts to help you know that your plastic surgeon is using the No Touch - No Pain technique in Breast Augmentation
Watch the testimonial and flawless recovery and correction achieved on this patient’s breasts after breast augmentation. The patient is comparing the No Touch - No Pain Technique used by Plastic Surgeon Evangelos Keramidas with the classic technique.
See all videos on breast augmentation.
 No Touch - No Pain - συνέντευξη στον ΣΚΑΪ στην εκπομπή Ζωή.gr της Χριστίνας Βίδου
No Touch - No Pain - συνέντευξη στον ΣΚΑΪ στην εκπομπή Ζωή.gr της Χριστίνας Βίδου Αυξητική Στήθους No Touch No Pain - 11ο Πανελλήνιο Συνέδριο Πλαστικής Χειρουργικής
Αυξητική Στήθους No Touch No Pain - 11ο Πανελλήνιο Συνέδριο Πλαστικής Χειρουργικής  Αυξητική Στήθους Νέα τεχνική χωρίς πόνο!
Αυξητική Στήθους Νέα τεχνική χωρίς πόνο! Πως να διαλέξουμε σωστά ενθέματα στην αυξητική στήθους
Πως να διαλέξουμε σωστά ενθέματα στην αυξητική στήθους  Αυξητική Στήθους No Touch No Pain - MEGA ΠΡΩΙΝΟ MOU
Αυξητική Στήθους No Touch No Pain - MEGA ΠΡΩΙΝΟ MOU Mega "Πρωϊνό mou" - Live χειρουργείο αυξητικής στήθους
Mega "Πρωϊνό mou" - Live χειρουργείο αυξητικής στήθους Αυξητική στήθους - Καταπληκτική ανάρρωση με τη νέα τεχνική
Αυξητική στήθους - Καταπληκτική ανάρρωση με τη νέα τεχνική Καταπληκτική ανάρρωση αμέσως μετά το χειρουργείο αυξητικής στήθους
Καταπληκτική ανάρρωση αμέσως μετά το χειρουργείο αυξητικής στήθους ΑΥΞΗΤΙΚΗ ΣΤΗΘΟΥΣ ΔΙΑΛΕΓΟΝΤΑΣ ΜΕΓΕΘΟΣ ΣΙΛΙΚΟΝΗΣ PART A
ΑΥΞΗΤΙΚΗ ΣΤΗΘΟΥΣ ΔΙΑΛΕΓΟΝΤΑΣ ΜΕΓΕΘΟΣ ΣΙΛΙΚΟΝΗΣ PART A ΑΥΞΗΤΙΚΗ ΣΤΗΘΟΥΣ ΔΙΑΛΕΓΟΝΤΑΣ ΜΕΓΕΘΟΣ ΣΙΛΙΚΟΝΗΣ PART B
ΑΥΞΗΤΙΚΗ ΣΤΗΘΟΥΣ ΔΙΑΛΕΓΟΝΤΑΣ ΜΕΓΕΘΟΣ ΣΙΛΙΚΟΝΗΣ PART B ΑΥΞΗΤΙΚΗ ΣΤΗΘΟΥΣ ΔΙΑΛΕΓΟΝΤΑΣ ΜΕΓΕΘΟΣ ΣΙΛΙΚΟΝΗΣ PART C
ΑΥΞΗΤΙΚΗ ΣΤΗΘΟΥΣ ΔΙΑΛΕΓΟΝΤΑΣ ΜΕΓΕΘΟΣ ΣΙΛΙΚΟΝΗΣ PART C Αυξητική Στήθους Η νέα No-Touch No-Pain Τεχνική
Αυξητική Στήθους Η νέα No-Touch No-Pain Τεχνική  Ρινοπλαστική βλεφαροπλαστική αυξητική στήθους
Ρινοπλαστική βλεφαροπλαστική αυξητική στήθους Ποιό ειναι το σωστό μέγεθος στην αυξητική μαστού
Ποιό ειναι το σωστό μέγεθος στην αυξητική μαστού Μάθετε τα πάντα για την αυξητική στήθους part 1
Μάθετε τα πάντα για την αυξητική στήθους part 1 Μάθετε τα πάντα για την αυξητική στήθους part 2
Μάθετε τα πάντα για την αυξητική στήθους part 2 Νέα μέθοδος αυξητικής στήθους No Touch-No Pain
Νέα μέθοδος αυξητικής στήθους No Touch-No Pain
Poster Award
Breast reduction is a procedure that aims at reducing the size and at the same time lifting the breasts. It also contributes in relieving the patient from intense pain in the chest and back caused by heavy breasts. Furthermore, it improves posture. Breast reduction may be performed at any age provided that the development of the breasts has been completed.
During the procedure, the breasts are reshaped so that the areola can be positioned in a more visible and higher level. Excess mammary gland and fat is reduced along with the skin from below the breast and from the sides. Also, if the areola has grown along with the overall enlargement of the breast, it will be reduced to match the size of the new breast. After surgery, that is performed with general anaesthesia, the patient remains in hospital for 1-2 days. Thin drainage tubes are inserted in each breast to prevent liquid/blood accumulation and are usually removed before discharge.
Scars, which usually heal well, are seen around and under the areola, in an inverted-T shape. Scars are also visible along the inframammary fold. Sometimes the procedure may be performed through an incision around the areola and a vertical incision under the areola. Scars are permanent and visible after the procedure, but they improve significantly over time. Depending on the size and shape of the breast, the procedure may be performed through a vertical incision thus avoiding the large horizontal incision. This is the “Lejour” technique or the vertical incision breast reduction procedure and can be performed only in specific cases.
After surgery, the patient is advised to wear a strong support bra for a month. Straight after the procedure, the breasts are bruised, swollen and a bit painful. The pain is easily managed with painkillers. In some cases, healing may be delayed, particularly in areas where much strain is exercised. Special care must be given to wound changing for a few weeks, until full healing is achieved.
Another complication, although rare, is the haematoma that usually occurs the first hours after surgery. Another operation is necessary to manage the situation. Inflammation is also a rare complication that is treated with appropriate antibiotics. Also, some patients may experience hypoesthesia in the area of the breasts, and oedema which usually subside over time. In very rare cases these complications may remain. Moreover, candidate patients should know that following breast reduction, it is possible that they will not be able to breastfeed although their breasts will continue to react (becoming bigger or smaller) to any changes occurring in their body (pregnancy, weight fluctuations, menopause).
Breast lift or mastopexy is a procedure used for changing the shape of breasts and simultaneously lifting the breasts. During the procedure, the breasts are reshaped so that the areola can be positioned in a more visible and higher level. Excess skin is removed from below the breast and from the side.
Also, if the areola has grown excessively following the overall laxity of the breast, it will be reduced to match the size of the new breast. After surgery, which is performed with general anaesthesia, the patient remains in hospital for one night.
Scars, which usually heal well, are seen around and under the areola, in an inverted-T shape. Scars are also visible along the inframammary fold. Sometimes the procedure may be performed through an incision around the areola and a vertical incision under the areola. Depending on the size and shape of the breast, the procedure may be performed through only one vertical incision. The large horizontal incision can be avoided.
Scars are permanent. Straight after surgery they are reddish and develop hard tissue, but they are smoothed out within a few months and their colour changes to match the skin’s tone. After a while they will only be slightly visible. Also, in some cases, if this is considered necessary, mastopexy can be combined with breast implant placement. The surgeon must co-operate with each patient in order to identify the appropriate technique.
After surgery, the patient is advised to wear a strong support bra for a month. Straight after the procedure, the breasts are bruised, swollen and a bit painful. The pain is easily managed with painkillers. Another complication, although rare, is haematoma that usually occurs the first hours after surgery. Another procedure is necessary to manage the situation.
Inflammation is also a rare complication that is treated with appropriate antibiotics. Also, some patients may experience hypoesthesia in the area of the breasts, and oedema which usually subside over time. In very rare cases these complications may remain. Moreover, interested patients must know that after breast reduction it is possible that they will not be able to breastfeed although their breasts will continue to react (becoming bigger or smaller) to any changes occurring in their body (pregnancy, weight fluctuations, menopause).
What is gynecomastia

Gynecomastia is the increase in size of male breasts due to hypertrophy and hyperplasia of the mammary tissue or fatty tissue (false gynecomastia) or both
Gynecomastia comes from the Greek words “gyne” and “mastos” which mean woman and breast, respectively and refers to any condition that causes excessive growth of the male breast tissue.
The male breast consists of the mammary gland and fat called adipose tissue. Patients with advanced gynecomastia have excess skin and sagging breasts.
Galen, the prominent Greek physician of the Roman Empire, was the first to use the word “gynecomastia” in the 2nd century AD to describe the unusual growth of male breast tissue.
Paul of Aegina, one of the pioneering physicians in Byzantium, described the first breast surgery for treating gynecomastia in the 7th century AD.
The problem
Patients who suffer from gynecomastia find no sympathy and feel ashamed and embarrassed.
Coaches, other kids, even parents may cause psychological trauma to patients with gynecomastia.
Patients must seek information about what exactly gynecomastia is and how they can handle the situation.
Gynecomastia therefore involves the increase in size of the male breast. The growing tissue may consist of the mammary gland or the fatty tissue or a combination thereof. Some cases may also involve excess skin as well as sagging breasts.
Pictures of Gynecomastia
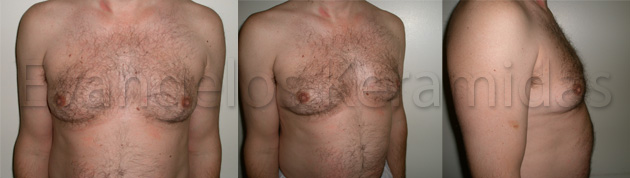


Patients present with enlarged breasts which are also asymmetric in 1/3 of cases. Some patients develop gynecomastia on one breast only.
There are 3 types of gynecomastia as per the Webster’s Classification (1934)
Type 1. Patients with enlarged mammary gland; treated through surgery.
Type 2. Patients with fatty tissue and enlarged mammary gland – pseudo gynecomastia – treatment through liposuction and surgery.
Type 3. This is type 1 and type 2 combined with excess skin.
Simon’s classification of gynecomastia (1973).
- Small yet visible increase of breast size
2a. Moderate increase of breast size but normal skin.
2b. Moderate increase of breast size and small degree of excess skin.
3 Very large breast. Breast ptosis. Large degree of excess skin.
Information
Reconstructive breast surgery offers bodily and psychological joy to a woman who has lost her breast either due to a mastectomy or due to any other condition (injury, burn, congenital abnormality).
It usually includes more than one surgical procedure performed at different stages. Reconstruction may begin along with mastectomy, or at a later stage, after the patient has recovered from radiotherapy.
 Ερ. Τον Ιούνιο του 2007 βραβεύτηκε στο Βερολίνο, στο Διεθνές Συνέδριο της Πλαστικής Χειρουργικής ανάμεσα σε 500 εργασίες απ’ όλο τον κόσμο, η εργασία σας “Composite Plane Breast Augmentation: A new Concept”. Σ’ αυτή παρουσιάζατε μία τελείως καινούργια τεχνική για την αυξητική μαστού.
Ερ. Τον Ιούνιο του 2007 βραβεύτηκε στο Βερολίνο, στο Διεθνές Συνέδριο της Πλαστικής Χειρουργικής ανάμεσα σε 500 εργασίες απ’ όλο τον κόσμο, η εργασία σας “Composite Plane Breast Augmentation: A new Concept”. Σ’ αυτή παρουσιάζατε μία τελείως καινούργια τεχνική για την αυξητική μαστού.
Η τεχνική αυτή είναι στην πραγματικότητα τροποποίηση της τεχνικής που παρουσίασε για πρώτη φορά ο Dr Tebbets από το Τέξας, ο γκουρού για μένα και μεγάλος δάσκαλος της αυξητικής του Μαστού.
Ερ. Τι ακριβώς είναι αυτή η τεχνική;
Μέχρι πρότινος ξέραμε δύο τεχνικές στην αυξητική μαστού, όσο αναφορά την τοποθέτηση του ενθέματος, την υπό του αδένος (subglandular) και υπό του μυός (submuscular). Το 2002 ήρθε να προστεθεί και η υποπεριτονιακή τεχνική (Sub Facial). Η δική μας τεχνική συνδυάζει τις δύο τελευταίες τεχνικές. Δηλαδή το ένθεμα σιλικόνης μπαίνει και κάτω από τον μυ και κάτω από την περιτονία του μυός.
Ερ. Νομίζω ότι ακούγεται λίγο μπερδεμένο
Στην πραγματικότητα δεν είναι. Κοιτάξτε το σχήμα 1. Το πάνω μέρος του ενθέματος σιλικόνης καλύπτεται από τον μείζωνα θωρακικό και το κάτω μέρος από την περιτονία του μυός (ένας λεπτός ιστός που καλύπτει τον μυ).
Ερ. Και γιατί να μην χρησιμοποιήσουμε τις παλαιές τεχνικές;
Γιατί καμία τεχνική δεν είναι τέλεια. Κάθε καινούργια τεχνική έρχεται για να προσφέρει κάτι καλύτερο.
Ερ. Εδώ λοιπόν ποια είναι τα πλεονεκτήματα και ποια τα μειονεκτήματα εάν βέβαια υπάρχουν.
Τα πλεονεκτήματα είναι πάρα πολλά:
1. Μειώνονται οι επιπλοκές, όπως του σχηματισμού της ρικνωτικής κάψας. Μια επιπλοκή που βασανίζει το 1-20% των γυναικών που έχουν υποστεί αυξητική του μαστού. Τοποθετώντας το ένθεμα κάτω από τον μυ και την περιτονία ελαχιστοποιούμε την επαφή του ενθέματος με τον μαστικό αδένα και αυτό πιθανολογείται ότι ελαττώνει το σχηματισμό της ρικνωτικής κάψας.
2. Φυσικότερο αποτέλεσμα ειδικά σε αδύνατους ασθενείς με ελάχιστο μαστό. Αυτό επιτυγχάνεται λόγω του ότι το άνω τμήμα του ενθέματος καλύπτεται από τον μυ.
3. Ελαττώνεται η πιθανότητα πτώσης του μαστού. Ο μυς και η περιτονία συγκρατούν το ένθεμα στη θέση του.
4. Αποφεύγουμε τις παραμορφώσεις που μπορεί να υποστεί το ένθεμα από την δύναμη του μείζονος θωρακικού όταν το ένθεμα τοποθετηθεί μόνο κάτω από τον μυ. Η λεγόμενη “open breast” ανωμαλία.
5. Ελαττώνεται η πιθανότητα ψηλάφησης των άκρων του ενθέματος.
6. Δεν σχηματίζονται ποτέ ρυτιδώσεις στο άνω μέρος του μαστού.
Ερ. Και τα μειονεκτήματα:
Μειονεκτήματα ουσιαστική δεν υπάρχουν, εκτός του ότι ο γιατρός χρειάζεται λίγο μεγαλύτερη εμπειρία για την εκτέλεση αυτής της τεχνικής.
Ερ. Χειρουργικά διαρκεί πιο πολύ σε σχέση με τις άλλες τεχνικές;
Όχι, σε έμπειρα χέρια διαρκεί ακριβώς το ίδιο από 30-45 λεπτά.
Ερ. Τοποθετείτε παροχέτευση, δηλαδή σωληνάκι στο μαστό;
Όχι, ούτε παροχετεύσεις ούτε επιδέσμους, ούτε ασφυκτικό κορσέ στον μαστό.
Ερ. Γιατί;
Εδώ ακριβώς εισέρχεται το πρώτο σκέλος του τίτλου αυτού του άρθρου.
Ερ. Δηλαδή το non-touch, no pain: τι σημαίνει;
Κυριολεκτικά σημαίνει δεν αγγίζω, δεν πονάει. Και εξηγούμε. Στη χειρουργική έχει μεγάλη σημασία το πώς συμπεριφέρεσαι τους ιστούς την ώρα που χειρουργείς. Όσο πιο πολύ τους σέβεσαι, δηλαδή δεν τους κακοποιείς και ακολουθείς τελείως ανατομικές και αναίμακτες τεχνικές, τόσο ελαχιστοποιείς τα προβλήματα μετά το χειρουργείο. Το ζητούμενο, σε μια κοινωνία που συνεχώς τρέχει σαν την δική μας, είναι η γρήγορη επάνοδος του ασθενούς στη φυσιολογική ζωή. Στόχος μας είναι ο ασθενής να μπορεί την ίδια μέρα μετά το χειρουργείο να είναι σε θέση να βγει για φαγητό και να πάει σινεμά.
Ερ. Και πως επιτυγχάνεται αυτό;
Χρησιμοποιώντας 1) ειδικά εργαλεία 2) τελείως ατραυματικές τεχνικές και 3) ειδικές ασκήσεις μετά το χειρουργείο
Με τον συνδυασμό των πιο πάνω επιτυγχάνουμε
1. Ταχύτητα ανάρρωσης
2. Στο 90% των ασθενών ο πόνος είναι ελάχιστος και μπορούν την ίδια μέρα να γευματίσουν έξω από το σπίτι τους
3. Όχι σωληνάκια
4. Όχι επιδέσμους στο στήθος
5. Όχι κορσέδες στο στήθος
6. Καθόλου μώλωπες (μελανιές) μετά την επέμβαση
7. Δραματική μείωση επιπλοκών όπως το αιμάτωμα και οι φλεγμονές.
Ερ. Ο συνδυασμός λοιπόν της ατραυματικής αυτής τεχνικής και του διπλού επιπέδου τεχνικής θα έχει ελαχιστοποιήσει ακόμα περισσότερο τα προβλήματα μετά το χειρουργείο;
Δραματικά. Οι επιπλοκές και οι επανεγχειρήσεις βρίσκονται αυτή τη στιγμή σ’ ένα ποσοστό μικρότερο του ένα τοις εκατό (1%). Ενώ το ποσοστό ικανοποίησης των γυναικών απ’ αυτή την επέμβαση αγγίζει το 98-99%, πράγμα που είναι και το ζητούμενο.
What is a tuberous breast
Tuberous Breast
The Tuberous or Tubular Breast is a congenital (from birth) abnormality of the breast shape. There are several theories that try to explain how this condition occurs, but the exact cause is yet unknown.
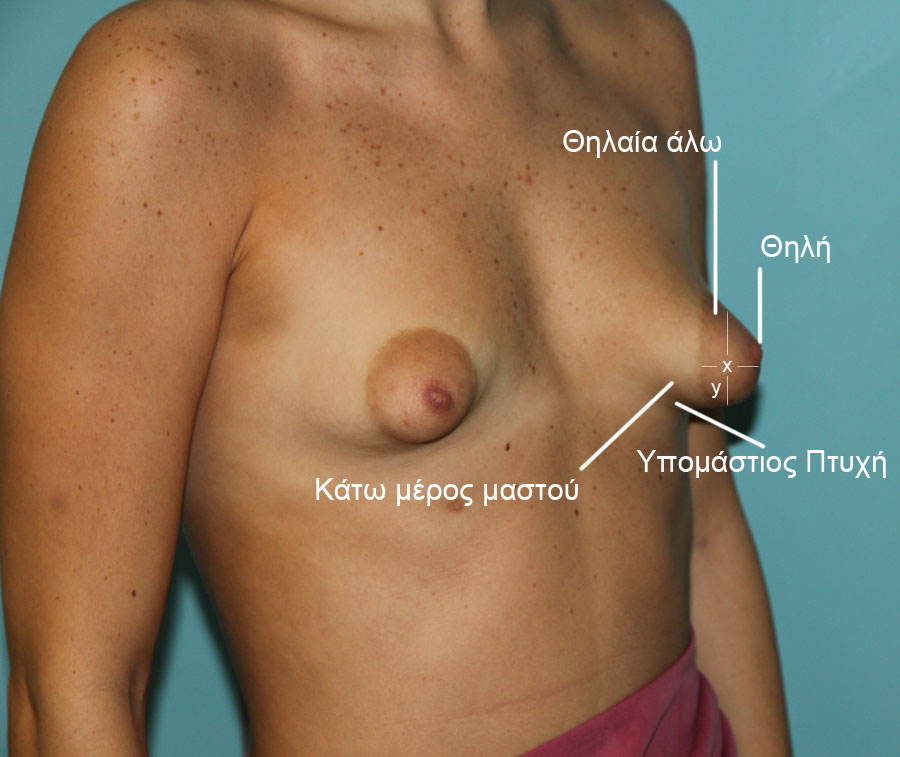
Normal Breast
The pictures below show a normal breast
The common features of tuberous breasts are:
1. Small (hypoplastic breast)
2. Enlarged and puffy areola.
3. Narrow base.
4. Higher than normal breast fold
5. Very small distance between the nipple and the breast fold.
6. Lower pole hypoplasia.
Other types of tuberous breasts
a. Hypoplastic tuberous breast with large and puffy areola
b. Breast asymmetry with funnel chest (pectus excavatum) and hypoplastic tuberous breast with areola of normal diameter
c. Sagging tuberous breast of normal volume
d. Great asymmetry of enlarged sagging tuberous breast
e. Breast asymmetry with normal chest and hypoplastic tuberous breast (Right)
Tuberous breast is rare in the general population. However, in patients who present for breast augmentation the numbers are much higher, reaching 30-40%.
In studies that we have carried out, in 2000 of our own patients who came to us for breast augmentation, tuberous breast reaches 33%.
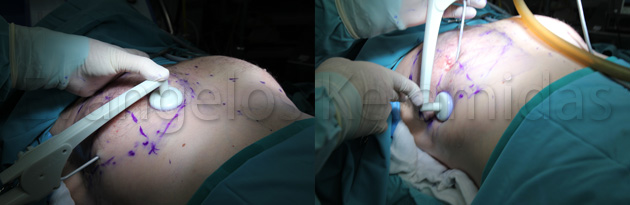
A new technique
It is very important for a patient to know that she has tuberous breasts. By identifying the condition of tuberous breasts on our patients we are able to plan the procedure in such a way as to avoid problems following breast augmentation. A patient with tuberous breasts must know that the breast(s) need(s) to be handled differently compared to a breast that is not tuberous.
Because of the difficulty in treating this problem, we propose a new combinatorial technique.
Our new technique was first presented at the ISAPS Geneva World Congress in September 2012.
To achieve a good result in tuberous hypoplastic breasts the following were necessary:
Firstly: To achieve good expansion of the breast’s lower pole
- Placement of silicone implants
- Incisions made internally at the breast’s lower pole (view photo)
- Good contact of silicone implants with the breast’s lower pole to allow the breast to expand upon constant pressure of the implant (MUST technique).
For this purpose, the appropriate technique is the MUST technique.
Secondly: To correct the areola when and if necessary
It is very important to decide when to correct the areola and when not. The success of this surgery depends exactly on this detail.
Our decision is based on the x/y ratio. “x” is distance 1 and “y” is distance “2”. When the x/y ratio is less than 0.3 we do not interfere with the areola. But when the ratio is greater than 0.3 then we fix the areola
How is the areola corrected?
With a periareolar incision we reduce the areola to the desired size and manage breast projection. For closing we use a special technique and CV-3 suture.
Conclusion
Tuberous breasts can be easy to fix when the deformity is diagnosed before surgery and when all appropriate measures are taken to correct it. The new technique involves:
- Correction of the areola, where and when needed (ratio X/Y>0.35)
(ATTENTION, THIS IS NOT ALWAYS NECESSARY!)
- The Must technique in placing silicone implant for better expansion of the lower pole of the breast
Adhering to the above principles we may expect a very good result.
Wrong treatment of tuberous breast
Take a look at what can happen when a tuberous breast is not properly handled
What went wrong?
In the first case the breast develops an excessive "double bubble deformity" due to failure to correct the problem
Effort to correct the areola diameter: if performed alone it fails to correct the deformity, and, if not performed correctly, it leads to further problems.
Take a look at the before and after pictures of tuberous breast surgeries
1) Capsular contracture

Α) A rare complication that may occur after breast augmentation.
We do not know its exact cause. The main hypothesis as to its cause and pathogenesis claims that this is a biological response to the implant (foreign body) leading to the formation of a capsular contracture around the implant. In capsular contracture, the reaction produces collagen fibres, fibroblasts and fibromyoblasts on the capsule. This becomes hard and is often painful.
Some factors such as subclinical inflammation, biofilm formation (bacteria on the implant surface), bleeding during surgery, incision location, implant pocket location, may increase the possibility of capsular contracture formation, however, there is no specific explanation as to its exact causes. Roughly, capsular contracture is classified in four Grades.
GRADE A : The patient does not feel anything but, during palpation, the doctor can identify tissue hardness.
GRADE B : Patient can feel a slight firmness of the breast.
GRADE C : The breast becomes firmer and starts to change in shape.
GRADE D : All above symptoms along with painful breast.
TREATMENT
The only treatment is surgical. 20 to 30 years ago, surgeons would try to break the capsule by pressing hard against the breast, but this technique is now strongly denounced.
EXAMPLE
Patient submitted to breast augmentation 5 years ago. She noticed that her left breast has started to change in shape and felt firmer. The patient’s implant was under the mammary gland.
SURGICAL APPROACH
1) Access through previous incision.
2) Implant removal.
3) Creation of new pocket beneath the pectoralis major muscle. (there are several indications suggesting that capsule formation is reduced when the implant is placed under the muscle.)
4) Use of rough surface implants (associated with less chances of capsular contraction.)
5) Suturing of the pocket.
6) Incision closure.
7) Result is full correction of the breasts.
8) How can we restrict capsular contracture:
- By placing the implant either under the muscle or by using the subfascial or dual plane technique
- Rough surface implants suggested most suitable
- Inframammary incision
- Non touch- No pain technique in surgery
- No bandages or tight bras or massage on the breasts after surgery
2) High-riding of implants
 Implants that are mispositioned higher than normal. Implants placed under the muscle can rarely be mispositioned higher up the chest.
Implants that are mispositioned higher than normal. Implants placed under the muscle can rarely be mispositioned higher up the chest.
Treatment
Example
Treatment is only surgical.
1) Planning of correct implant position.
2) Access through previous incision
3) Implant removal (no need to change the implant)
4) Preparation of down-facing pocket if needed
5) Implant placement
6) Suture
7) Results
3) Tuberous Breast

What is a tuberous breast?
The Tuberous or Tubular Breast is a congenital (birth) abnormality of the breast shape. There are several theories that try to explain how this condition occurs, but the exact cause is yet unknown.
Example
Patient submitted to breast augmentation.
Case: Patient with non-identified tuberous breast is seen with 1) double-bubble deformity 2) large areola 3) pocket deformity.
Surgical approach
This is among the toughest cases we are called to treat
Surgery stages - diagnosis
Problems
1) Pocket
2) Lower quadrant of the breast
3) Areola
Surgical treatment
1) Incision around the areola – periareolar
2) Implant replacement
3) Pocket change from inframammary to M.U.S.T.
4) Release of entire breast
5) Vertical and horizontal lines to expand the inferior segment of the breast as this is a tuberous breast case

6) Placement of new implants
7) Lifting and correction of the areola with a special technique, the “tobacco pouch” and special permanent suture CV-3
8) Correction of right breast on the operating table
9) Left breast is not yet corrected
10) Same procedure is repeated for left breast
11) Correction of both breasts
12) First day post-op. Red-orange stain is Betadine
13) 6 months post-op
14) Results at 8 months post-op
15) Result comparison
Read more about tuberous breasts here
4) Double-bubble
 A rare complication seen following breast augmentation. Patients present with two parallel, transverse and curved folds along the lower pole of the breast that correspond to the breast and the silicon implant. Although the cause of this complication is yet to be clarified, surgeons believe that this is due to either a downward shifting of the implant, a capsular contraction or a ptosis of the breast. It is more often seen in cases of tuberous breasts, small breasts with disproportionately large implants, breasts with small areola to inframammary fold distance, breasts with large inframammary fold. There are several ways to correct this malformation. The most popular approach is capsulorraphy that allows the implant to shift to a normal position.
A rare complication seen following breast augmentation. Patients present with two parallel, transverse and curved folds along the lower pole of the breast that correspond to the breast and the silicon implant. Although the cause of this complication is yet to be clarified, surgeons believe that this is due to either a downward shifting of the implant, a capsular contraction or a ptosis of the breast. It is more often seen in cases of tuberous breasts, small breasts with disproportionately large implants, breasts with small areola to inframammary fold distance, breasts with large inframammary fold. There are several ways to correct this malformation. The most popular approach is capsulorraphy that allows the implant to shift to a normal position.
EXAMPLE
35-year-ole patient with double-bubble deformity following left breast augmentation.
TREATMENT
1) Planning of new implant position.
2) Access through previous incision.
3) Implant removal
4) Capsule suture with permanent internal stitches and restriction of previously enlarged area.
5) Result correction.
Another way to correct the double-bubble deformity is to create a new pocket between the pectoralis major and the anterior capsule. We then close the old pocket with stitches and place the implant in the new pocket.
3 Months after






 No Touch - No Pain - συνέντευξη στον ΣΚΑΪ στην εκπομπή Ζωή.gr της Χριστίνας Βίδου
No Touch - No Pain - συνέντευξη στον ΣΚΑΪ στην εκπομπή Ζωή.gr της Χριστίνας Βίδου Αυξητική Στήθους No Touch No Pain - 11ο Πανελλήνιο Συνέδριο Πλαστικής Χειρουργικής
Αυξητική Στήθους No Touch No Pain - 11ο Πανελλήνιο Συνέδριο Πλαστικής Χειρουργικής  Αυξητική Στήθους Νέα τεχνική χωρίς πόνο!
Αυξητική Στήθους Νέα τεχνική χωρίς πόνο! Πως να διαλέξουμε σωστά ενθέματα στην αυξητική στήθους
Πως να διαλέξουμε σωστά ενθέματα στην αυξητική στήθους  Αυξητική Στήθους No Touch No Pain - MEGA ΠΡΩΙΝΟ MOU
Αυξητική Στήθους No Touch No Pain - MEGA ΠΡΩΙΝΟ MOU Mega "Πρωϊνό mou" - Live χειρουργείο αυξητικής στήθους
Mega "Πρωϊνό mou" - Live χειρουργείο αυξητικής στήθους Αυξητική στήθους - Καταπληκτική ανάρρωση με τη νέα τεχνική
Αυξητική στήθους - Καταπληκτική ανάρρωση με τη νέα τεχνική Καταπληκτική ανάρρωση αμέσως μετά το χειρουργείο αυξητικής στήθους
Καταπληκτική ανάρρωση αμέσως μετά το χειρουργείο αυξητικής στήθους ΑΥΞΗΤΙΚΗ ΣΤΗΘΟΥΣ ΔΙΑΛΕΓΟΝΤΑΣ ΜΕΓΕΘΟΣ ΣΙΛΙΚΟΝΗΣ PART A
ΑΥΞΗΤΙΚΗ ΣΤΗΘΟΥΣ ΔΙΑΛΕΓΟΝΤΑΣ ΜΕΓΕΘΟΣ ΣΙΛΙΚΟΝΗΣ PART A ΑΥΞΗΤΙΚΗ ΣΤΗΘΟΥΣ ΔΙΑΛΕΓΟΝΤΑΣ ΜΕΓΕΘΟΣ ΣΙΛΙΚΟΝΗΣ PART B
ΑΥΞΗΤΙΚΗ ΣΤΗΘΟΥΣ ΔΙΑΛΕΓΟΝΤΑΣ ΜΕΓΕΘΟΣ ΣΙΛΙΚΟΝΗΣ PART B ΑΥΞΗΤΙΚΗ ΣΤΗΘΟΥΣ ΔΙΑΛΕΓΟΝΤΑΣ ΜΕΓΕΘΟΣ ΣΙΛΙΚΟΝΗΣ PART C
ΑΥΞΗΤΙΚΗ ΣΤΗΘΟΥΣ ΔΙΑΛΕΓΟΝΤΑΣ ΜΕΓΕΘΟΣ ΣΙΛΙΚΟΝΗΣ PART C Αυξητική Στήθους Η νέα No-Touch No-Pain Τεχνική
Αυξητική Στήθους Η νέα No-Touch No-Pain Τεχνική  Ρινοπλαστική βλεφαροπλαστική αυξητική στήθους
Ρινοπλαστική βλεφαροπλαστική αυξητική στήθους Ποιό ειναι το σωστό μέγεθος στην αυξητική μαστού
Ποιό ειναι το σωστό μέγεθος στην αυξητική μαστού Μάθετε τα πάντα για την αυξητική στήθους part 1
Μάθετε τα πάντα για την αυξητική στήθους part 1 Μάθετε τα πάντα για την αυξητική στήθους part 2
Μάθετε τα πάντα για την αυξητική στήθους part 2 Νέα μέθοδος αυξητικής στήθους No Touch-No Pain
Νέα μέθοδος αυξητικής στήθους No Touch-No Pain

 What is the SubFascial technique?
What is the SubFascial technique?











 Send us your questions
Send us your questions




























Follow us

